A validation master plan (VMP) details all the vital elements for effectively validating production processes, such as the approach, activities, and strategy of an organization. If you’re seeking ISO 13485 certification, the VMP supports this by ensuring that any alterations or deviations are controlled effectively, and it emphasizes the importance of maintaining consistency in your product’s quality. But is a VMP mandatory as part of ISO 13485 accreditation? Let’s find out.
According to ISO 13485, manufacturers must validate any processes involved in production and service provision, particularly when the final output cannot be verified by later monitoring or measurement. The validation master plan is one way to achieve that, and it outlines a systematic approach to validation to meet pre-defined quality specifications.
Which processes need validation?
Process validation is a systematic approach that establishes whether a given process consistently produces a product that meets predefined quality specifications. Validation is necessary only for processes whereby results cannot be observed by the naked eye, and it serves as a method of providing objective evidence of this.
Examples of processes that need validation
- Sterilization – it’s not possible to see if the product is sterile after the sterilization process has been carried out.
- Cleanroom management – these limit airborne particles, such as dust and microbes, but it’s impossible to see how many of these particles are in the air.
Examples of processes that do not need validation
- Metal and plastic processing – you can visually confirm adherence to shape and dimension specifications for medical devices, which can also be measured.
- Labeling – visually inspecting the labels to ensure that they are applied correctly, and that they contain the necessary information, is usually straightforward.
For such processes, validation ensures that the end product will possess the necessary characteristics when the correct procedure is conducted with the designated equipment.
Do I need a VMP under ISO 13485?
ISO 13485 doesn’t explicitly require a validation master plan. However, in clause 7.5.2, the standard mandates planning for product realization.
In essence, you cannot properly plan production where reproducibility of the process cannot be shown, and where every single process takes place exactly as prescribed. As such, a well-structured VMP could potentially form a necessary part of this planning process.
To learn more, read Using ISO 13485 to manage process validation in the medical device manufacturing industry.
The two types of validation
There are two main types of process validation that ensure continued quality throughout a product’s lifecycle:
- Initial validation takes place when the system or procedure is first introduced.
- Revalidation follows changes that potentially impact the product’s quality, such as modifications in the raw materials, equipment, system software, facilities, or support systems.
Revalidation is also carried out periodically, even in the absence of changes, to ensure that the process remains in a state of control.
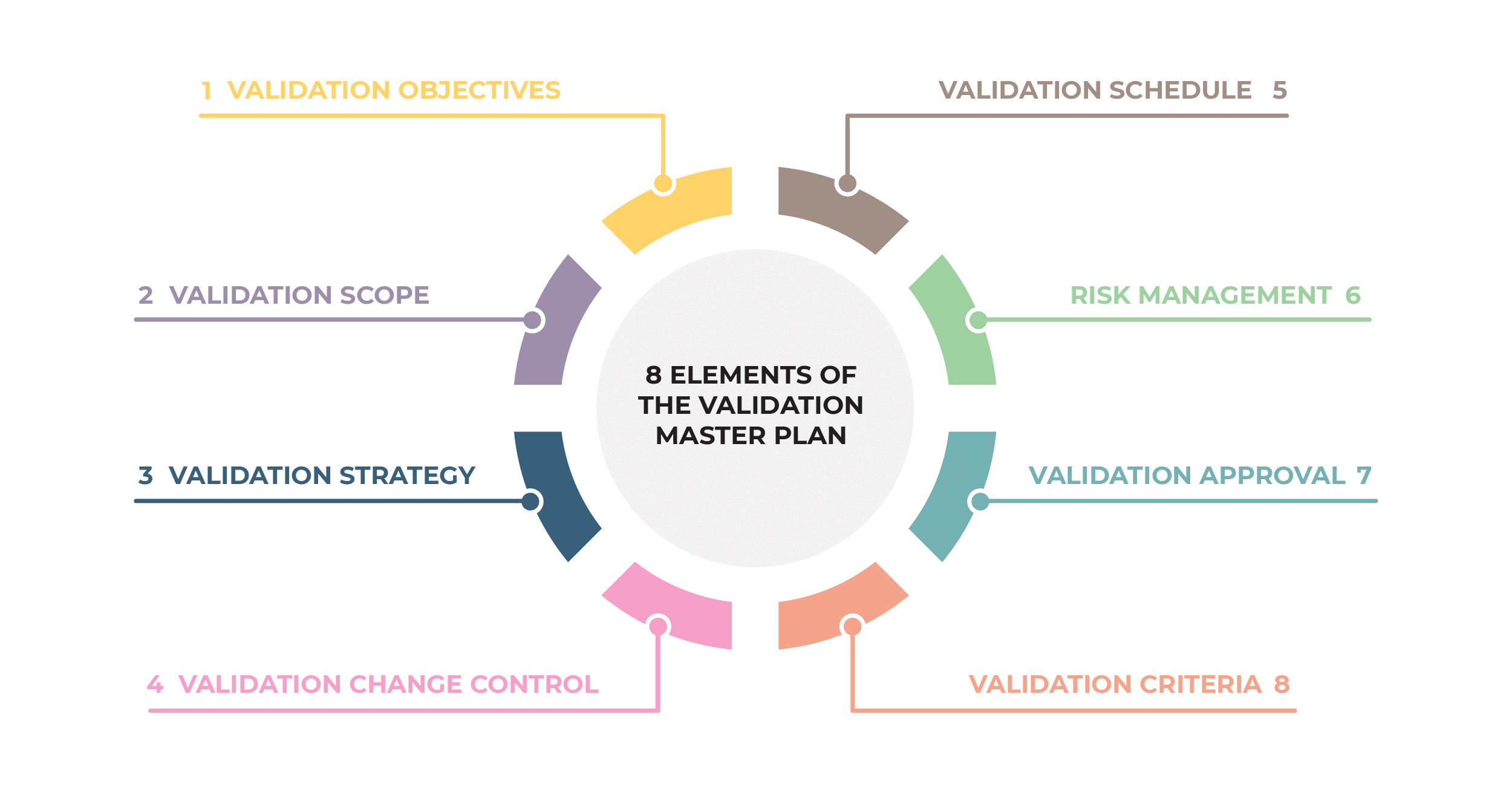
Eight elements of the validation master plan
The validation master plan serves as a blueprint for ensuring that the device is both safe and effective for its intended use. It includes the testing and evaluation methods to be used, the data to be collected, the standards to be met, and the criteria for evaluating the results.
The key elements of the VMP are included below using the example of dental implants.
See here for more information: How to manage medical device sterilization according to ISO 13485.
1. Validation objectives
The validation objectives are the first things that need to be defined as part of the VMP. They outline what needs to be accomplished through this process. This could involve initial validation when a process is introduced, or revalidation.
Here’s an example objective relating to dental implant sterilization.
2. Validation scope
The next element in the VMP is the validation scope. Manufacturers should describe the specific product and its intended purpose, as well as the associated facilities, systems, equipment, and processes.
For instance, the dental implant manufacturer will specify the facility’s address where sterilization will be conducted, identify the appropriate sterilizer (by the type, name, and mark), and describe the type of sterilization pouch (with defined specifications and declarations).
3. Validation strategy
After determining the scope, the validation strategy is outlined. It must distinctly delegate roles and responsibilities on both personal and institutional levels.
For dental implant sterilization, it would be necessary to stipulate the following personnel and their respective responsibilities:
- the quality manager and the part of the validation they coordinate
- the operative who carries out the sterilization process itself
- the person responsible for the maintenance of the sterilizer
- the production manager who will produce and package the requested medical products
If the testing is to be outsourced, specify the institution where these tests will be performed, as well as the responsible person in that institution. The strategy should also include a section dedicated to applicable references to the procedures and work instructions from the manufacturer’s Quality Management System (QMS).
4. Validation change control
The VMP must define the change control process for the validation program and list the required deliverables, ensuring alignment with the organization’s QMS. If there is any change from what was planned during the validation process, the following must be documented:
- How will these changes be managed?
- Who is responsible for approving the changes?
- What impact will these changes have on other aspects of validation?
A dental implant manufacturer may have started the validation using a particular type of dental implant, only to switch to a different type of implant as the validation progresses. This would need to be addressed as part of the change control activity.
5. Validation schedule
After the change control has been established, a detailed timeline for each validation activity must be outlined. At this stage, it’s necessary to list every activity that needs to be completed during the validation process.
For a dental implant manufacturer, this could include scheduling these activities:
- sterilization of dental implants
- post-sterilization testing
- data collection and analysis
- report writing
- review and approval processes
Next is to determine how long each activity is likely to take. Be realistic and allow for unexpected delays. Some activities will need to be completed before others can begin. Also, defining responsibilities for each activity and mapping out the activities will ensure accountability.
6. Risk management
After the scheduling of validation tasks, a risk assessment must be carried out to identify risks associated with the processes, systems, and equipment. This is critical in preventing issues that could compromise the quality of the products or the compliance of the process.
Risks associated with the production of dental implants could include:
- Inadequate sterilization after manufacturing could lead to infections.
- Residual oils and chemicals could potentially cause allergies or toxicity.
- Poorly processed implants might be excessively sharp.
Once these risks are identified, strategies to mitigate them should be integrated into the validation plan.
7. Validation approval
After the risk assessment has been carried out, management’s approval and commitment should be secured to ensure that the plan has the support to be implemented. This could involve acquiring the signatures of individuals such as:
- quality management representatives
- validation engineers
- senior management
The exact approval process will vary depending on the structure of the organization, regulatory requirements, and the complexity of the medical device. Adopting a collaborative approach to writing VMPs is beneficial, as it incorporates knowledge from different operational areas, ensuring that all processes, utilities, equipment, and systems are considered.
8. Validation criteria
After approval has been signed off, the validation master plan should outline the expected outcomes of the validation, that is, the acceptable criteria. For each test conducted, predetermined acceptable and unacceptable results should be clearly defined.
In the case of sterilization, acceptable results would be the sterility of the dental implants, as evidenced by a negative result from sterile biological indicators.
Validating ISO 13485 compliance
A well-structured validation master plan ensures consistent production of safe and effective medical devices, a key requirement of ISO 13485. Through it, manufacturers can demonstrate control over the reproducibility of their products and effectively manage any changes in the process, to ensure continuous compliance with the standard through revalidation.
See our ISO 13485 Integrated Documentation Toolkit for step-by-step guidance and unlimited access to all document templates required for IS0 13485 certification.

 Kristina Zvonar Brkic
Kristina Zvonar Brkic